Climate change isn’t a distant threat. It’s here, and it’s hitting harder than ever—especially when it comes to human health. As global temperatures rise, ecosystems are shifting faster than our systems can adapt. Mosquito-borne diseases like dengue and malaria are showing up in places they rarely touched before. Smoke from wildfires is polluting air hundreds of miles away. Heatwaves are pushing hospitals to capacity.
This isn’t just about polar bears or sea levels anymore. Climate change is triggering real-time health emergencies, and communities around the world are feeling it. From respiratory issues in cities choked with smog to mental health struggles tied to displacement and disaster, the impacts are personal—and multiplying.
Public health experts are sounding the alarm, and so are doctors on the ground. The message is clear: stop treating climate as a siloed environmental problem. It’s a medical crisis, a mental health challenge, and a threat multiplier. Rising temperatures don’t just change the weather; they reshape the way we live, breathe, and survive.
Climate Change is Expanding the Reach of Disease-Carrying Insects
As global temperatures rise, the habitats of insects that transmit diseases are shifting. This is not just a future concern—it is a growing reality impacting public health around the world.
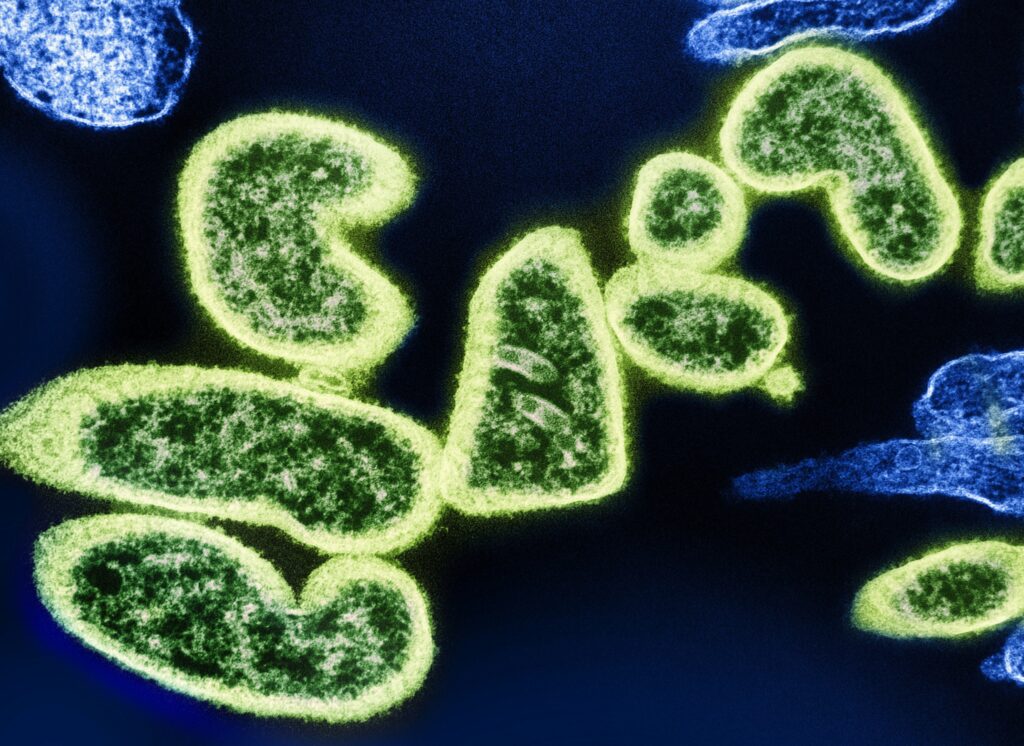
Insects on the Move
Warmer climates are enabling disease-carrying insects to survive in places that were previously too cold for them.
- Mosquitoes are thriving in higher altitudes and latitudes
- Ticks are expanding into new territories, including parts of Europe and North America
- These shifts increase the risk of insect-borne illnesses in areas historically unexposed to them
Rising Cases in New Regions
Communities that once had no need to worry about certain diseases are now seeing increasing numbers of infections.
- Dengue fever is appearing in regions previously unaffected, including Southern Europe and the Southern United States
- Malaria cases are on the rise outside traditional tropical zones
- Lyme disease is spreading further north due to longer warm seasons
Healthcare Under Pressure
The spread of these diseases places growing pressure on global healthcare systems, especially in low- and middle-income countries.
- Limited resources make it difficult to diagnose and treat emerging diseases quickly
- Public health agencies must now adapt to new prevention and treatment strategies
- Preparedness efforts are often underfunded or lack local context
These changes underscore the need for stronger disease surveillance, improved vector control strategies, and adaptive health policies that reflect the realities of a warming climate.
Extreme heat isn’t rare anymore. It’s normal. Summer spikes that used to hit once a decade are now happening every couple of years, sometimes back-to-back. The sheer frequency of these heatwaves is rewriting what’s considered seasonally typical in huge parts of the world.
The health effects are serious. High temperatures put heavy stress on both the cardiovascular and respiratory systems. People with heart conditions, asthma, or even just mild respiratory issues feel the pressure first. Hospitals report more admissions during heatwaves, especially in urban areas where concrete traps heat overnight.
But the burden isn’t shared equally. The elderly, young children, and anyone working outside—construction crews, farm laborers, delivery drivers—are at the front lines. These groups often can’t escape the heat, and many lack access to cooling systems or healthcare support. For them, extreme heat is more than uncomfortable. It’s dangerous.
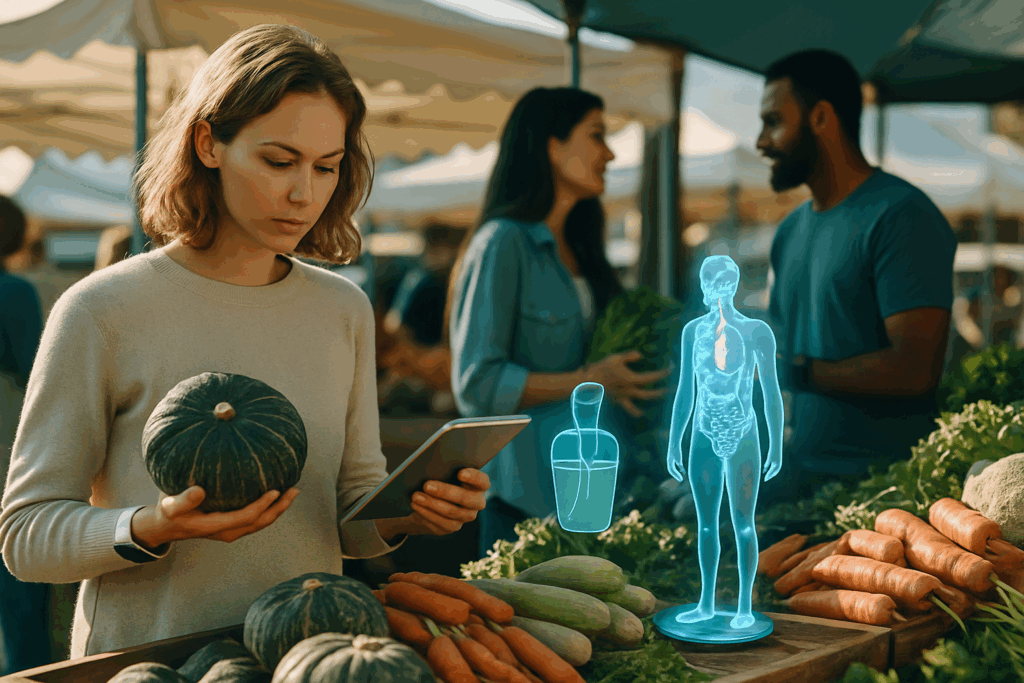
Climate change isn’t a distant threat anymore. One of its sharpest impacts hits the plate and the glass. Unpredictable weather—floods, droughts, late frosts—has led to real crop failures across regions that rely on consistent growing seasons. For communities dependent on local agriculture, this means less food and lower nutritional quality, especially among children.
Water isn’t fairing any better. As rain patterns shift and infrastructure struggles, contaminated drinking water has become a fast-growing health risk. Rural areas tend to be hit harder due to limited purification systems, while urban settings face aging pipes and overburdened treatment plants. Either way, the outbreaks of waterborne illnesses are no longer isolated stories—they’re patterns.
Access gaps between urban and rural areas are widening. Cities often have more resources, but that doesn’t guarantee safety or availability. In rural regions, long distances to reliable food and water sources make things worse. This divide means preparedness and policy need to be hyper-local. The impact of climate on health doesn’t play out evenly—it’s shaped by geography, infrastructure, and income.
Air quality is getting worse — not just in headlines, but in daily life. Vloggers shooting outdoors are dealing with more than bad lighting. Wildfire smoke, industrial emissions, and rising fine particle exposure now shape the backdrop of content — and health. These airborne pollutants aren’t just a nuisance. They’re strongly linked to spikes in asthma, allergies, bronchitis, and other respiratory conditions. Even short bursts of exposure can trigger long-term effects if left unchecked.
Urban areas are bearing the brunt of it. Smog layers the skyline in many cities, but the real damage happens inside the body. Fine particulate matter digs deep into the lungs and sneaks into the bloodstream, increasing the risk of heart disease over time. For creators who vlog in traffic-heavy or industrial neighborhoods, it’s not just a visual downgrade — it’s a health cost.
Staying aware of air conditions and planning around them isn’t optional anymore. It’s part of how creators protect themselves and their craft.
Mental Health Impacts of the Climate Crisis
The emotional toll of climate change is no longer a side note. It’s central. People aren’t just reading headlines about wildfires, floods, or droughts — they’re living through them. Climate anxiety is rising fast, especially among younger generations who feel like they’re inheriting a breaking planet with no clear path forward. But it goes deeper than worry. Real disasters bring real trauma: losing a home to a hurricane, watching crops fail, evacuating with no return date.
Displacement brings its own kind of instability. When people lose homes, jobs, or ties to a rooted community, the mental fallout is deep and long lasting. Depression, PTSD, and chronic stress are climbing around each wave of extreme weather. These aren’t abstract risks. They’re happening now, especially in regions hit first and hardest — places with the least support.
In much of the global south, mental health infrastructure is thin or non-existent. That creates a gap between need and care that keeps growing. Community support networks help, but often they’re also stretched, displaced, or overwhelmed. Climate impacts aren’t just environmental. They’re social, emotional, and deeply personal. Until the mental piece is addressed, solutions will stay partial.
Climate change isn’t a distant threat anymore. It’s showing up in ERs across the country. Floodwaters, heatwaves, wildfires—each event is sending waves of patients into emergency care, often overwhelming systems that were already stretched thin. Hospitals are dealing with more respiratory issues, trauma cases, medication disruptions, and displaced patients, all at once.
Beyond the human toll, infrastructure is taking a beating. Storms knock out power grids. Floods render entire facilities inaccessible. These aren’t one-off incidents—they’re stacking up and exposing how brittle parts of our healthcare backbone really are.
That’s forcing a conversation that’s long overdue: we need resilient care systems that don’t just react, but anticipate. Communities are beginning to invest in mobile clinics, decentralized care hubs, and early-warning tech to better prepare for surges. The future of healthcare isn’t just about high-powered machines and specialists—it’s about making sure care still happens when the lights go out.
Explore innovative responses here: Breakthrough Innovations in Preventive Healthcare.
Building Climate-Resilient Healthcare: What That Really Means
Climate change is no longer a distant threat. It’s already disrupting how we deliver healthcare—through extreme weather events, disease outbreaks, supply chain breakdowns, and infrastructure collapse. Building climate-resilient healthcare means designing systems that can adapt in real time. It means hospitals that can handle heatwaves and floods. Clinics that stay operational during blackouts. Supply chains that don’t crumble during storms.
Strengthening public health surveillance and early warning systems is one of the smartest plays we can make. When data flows smoothly—from hospital records to weather alerts to community-level sensors—governments can track disease patterns, spot emerging risks, and snap into action faster. AI and machine learning can support this, but the human coordination behind it has to be solid.
Policy matters, too. We need stronger frameworks to protect people most at risk. That includes funding for medical facilities in low-resource areas, insurance systems that work under stress, and emergency plans that prioritize the underserved. No flashy tech can replace leadership that sees where things are breaking and moves to fix them.
In the end, climate change is a health crisis. Fighting it is just as much about clean air and safe homes as it is about vaccines and hospital beds. Resilient healthcare isn’t a luxury anymore. It’s a necessity.
Climate change isn’t some far-off threat—it’s already changing how and where people get sick. Rising temperatures are shifting the range of disease-carrying insects like mosquitoes and ticks. Storms and flooding are contaminating water supplies. Air quality is getting worse, and that hits people with asthma or heart issues right now.
These impacts aren’t playing out evenly. Some regions are facing a faster wave of health stress—vector diseases in places that never had them, food insecurity where growing seasons are breaking down, mental health pressure as climate anxiety climbs. This isn’t 2050-talk. It’s happening in today’s emergency rooms and clinics.
If you’re paying attention, this isn’t about panic. It’s about being ready. Healthcare systems are starting to plan for climate-linked shifts in disease. Communities are adapting. But individuals need to stay dialed in, too. Knowing what’s moving, what’s rising, and what your local risks are makes a real difference. Awareness is step one. Action follows.