The Rise of DIY Health Monitoring
Health Testing Goes Personal
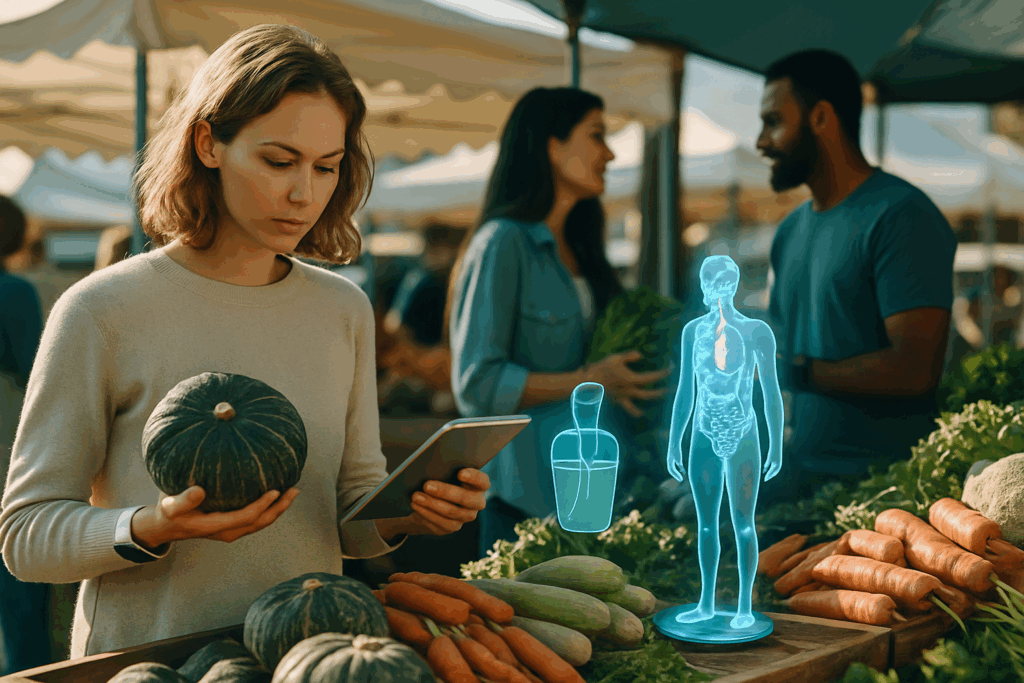
We’re seeing a major shift in how health data is collected. Traditional, clinic-based testing is giving way to decentralized, patient-controlled options. Consumers are no longer waiting for appointments or lab results—they’re taking matters into their own hands.
- At-home test kits are becoming mainstream
- Patients have more control over when and how they get tested
- Health data can now be monitored continuously, not just at checkups
This change is part of a broader movement toward personal empowerment in healthcare.
From Smart Devices to Full Diagnostic Tools
What began with fitness trackers and smart thermometers has evolved into more complex diagnostic solutions.
- Connected thermometers track fever trends across regions
- At-home blood tests and saliva diagnostics offer insights on everything from cholesterol to hormone levels
- Wearables monitor vitals like heart rate variability and oxygen saturation with clinical-level accuracy
These tools are moving beyond wellness tracking to real medical relevance.
Benefits and Limitations
While DIY health monitoring offers clear advantages, it’s not without trade-offs.
Pros:
- Faster access to personal health information
- Reduced burden on healthcare systems
- Better engagement in long-term wellness and preventive care
Cons:
- Risk of misinterpretation without medical guidance
- Privacy concerns with third-party health data platforms
- Accuracy and calibration can vary between at-home devices
As more people rely on self-monitoring tools, medical professionals and tech developers must work together to ensure accuracy, accessibility, and responsible use.
Redefining Healthcare: From Reactive Treatment to Proactive Prevention
The old model of healthcare was simple: wait until something breaks, then try to fix it. But that approach is getting replaced. Fast. Instead of reacting to illness, more systems are prioritizing early detection and preventive action. Why? Because it’s cheaper, faster, and avoids a lot of unnecessary suffering.
Governments and major health organizations are retooling their strategies to focus on prevention as the first line of defense. From regular screenings to digital health tracking, there is a growing push to stop problems before they start. This isn’t just a trend. It’s becoming policy.
And the numbers make it clear. Catching diabetes early, for example, can cut long-term costs by thousands per patient. Identifying mental health conditions before they escalate can save not only money but lives. Prevention leads to better outcomes and puts less strain on already overburdened systems.
We’re moving beyond the idea that medicine starts with a diagnosis. In 2024 and beyond, staying healthy begins with staying ahead.
Machine learning is becoming a quiet force in healthcare, identifying red flags long before any symptoms show up. It’s not magic. Algorithms process insane amounts of data from sources like medical histories, blood panels, genetic sequences, and even wearable sensor data. The patterns they detect aren’t something a doctor would see at a glance—but they matter.
Take wearables. They’re not just tracking steps and sleep anymore. Machine learning can analyze heart rate variability, temperature shifts, or changes in oxygen saturation and spot subtle deviations that signal higher risk for chronic conditions. Add patient history and genetic profiling to the mix, and it becomes a powerful early-warning system.
This isn’t about predicting doom. It’s about smarter prevention. If your data shows elevated risk for something like type 2 diabetes or heart disease, the system tailors advice for you: specific lifestyle tweaks, screenings, even nudges to adjust your exercise routine. Personalized prevention backed by data is no longer theory. Algorithms are already guiding daily decisions for thousands, and that number’s only going up.
The Microbiome’s Role in Chronic Disease Prevention
The Microbiome-Health Connection
Research continues to affirm that the gut microbiome plays a major role in preventing and managing chronic diseases. From autoimmune disorders to metabolic syndrome, the balance of bacteria in the digestive system is increasingly viewed as a critical indicator of overall health.
- A diverse gut microbiome is linked to lower levels of inflammation
- Imbalances have been associated with conditions like type 2 diabetes, obesity, and cardiovascular disease
- Microbial composition can influence immune system regulation and even mental health
Advances in Microbiome Testing and Personalization
New testing methods have taken gut health analysis to the next level. Microbiome kits now offer more accurate and user-friendly tools to assess bacterial diversity and give personalized dietary feedback.
- At-home microbiome tests provide accessible insights into gut health
- Data-driven recommendations connect food choices to individual microbial profiles
- Use of prebiotics and probiotics is becoming more targeted and science-backed
These innovations make it easier for individuals and practitioners to translate microbiome data into actionable steps that support long-term wellness.
Food as Medicine: A Precision-Based Approach
The idea of “food as medicine” has gained scientific traction thanks to microbiome science. Nutrition strategies are now being tailored not only to lifestyle but also to the unique bacterial composition of each person’s gut.
- Diets rich in fiber, fermented foods, and polyphenols support microbial diversity
- Research suggests certain dietary patterns can shift the microbiome toward a disease-resistant state
- Personalized nutrition plans are emerging as complementary tools in chronic disease management
Beyond the Hype: Grounding Microbiome Science
While the promise of gut health is exciting, it is important to separate fact from marketing. The microbiome field is still evolving, and not all claims are backed by robust evidence.
- Some commercial products overstate benefits
- Long-term clinical trials are still limited in some areas
- Consumers should seek guidance from qualified health professionals before making major changes
The science is strong, but nuanced. For those committed to long-term health, understanding and supporting the microbiome remains one of the most promising and practical strategies.
Fast-track vaccine platforms aren’t just a pandemic-era experiment—they’re becoming a cornerstone of how we fight disease. The mRNA playbook, originally built for speed during COVID-19, has cracked open new possibilities. Researchers are now aiming that same tech at tough targets like influenza, RSV, HIV, and even cancer. What once took years in the lab is now moving from concept to clinical trial in months.
But progress isn’t just about the science. Public trust still lags, especially for technologies that feel new or rushed. Education needs to catch up, and conversations around transparency are more important than ever. Regulation, while improving, remains a bottleneck in many countries. The balance is delicate: go too fast, people worry. Go too slow, lives are lost.
This isn’t just medical innovation—it’s a fundamental shift in how quickly humanity can respond to complex health threats. If the hurdles can be cleared, the timeline from lab bench to public benefit could look very different in the next decade.
A new playbook is emerging in the fight against drug-resistant bacteria. With traditional antibiotics losing their edge, researchers are doubling down on proactive defenses instead of just reactive fixes. The focus now is prevention, not just treatment.
One big shift: vaccines tailored to specific bacterial threats. These aren’t your flu season regulars. We’re talking targeted immunizations for hospital-acquired infections and even gut flora imbalances. Alongside that, bacteriophage therapy — viruses that hunt and kill bacteria — is finally escaping lab trials and moving toward frontline care. This approach offers precision without collateral damage to the body’s good bacteria.
Researchers are also testing new alternatives like antimicrobial peptides and CRISPR-based gene edits to disarm bacteria before they take hold. These strategies aim to block infection before it starts, sidestepping resistance problems entirely.
The message for clinicians and public health pros? The best way to treat a superbug may be to stop it from ever getting a foothold.
Learn more: What You Need to Know About Emerging Superbugs
Preventive Gene Editing: Theoretical or Inevitable?
Preventive gene editing isn’t sci-fi anymore. Tools like CRISPR have moved from petri dishes to policy debates. We’re no longer asking if we can prevent disease at the genetic level—we’re asking when. For conditions with strong genetic markers, editing embryos or treating individuals pre-symptom could rewrite how we define healthcare. Critics call it risky, but the science is catching up to the ambition. While ethical lines are still blurry, countries at the biotech frontier are already sketching out guidelines.
At the same time, tech-enabled public health initiatives are scaling like never before. Mobile diagnostics, AI-driven surveillance, and real-time data dashboards are linking urban clinics to rural outposts. Countries like Rwanda and India are experimenting at national levels. The goal: catch problems before they spread, quietly and efficiently.
Prevention today isn’t about luxury. It’s about avoiding collapse. Whether editing genes or deploying rapid-alert systems, global public health is shifting from response mode to preemption. And that makes prevention less a trend and more a survival strategy.